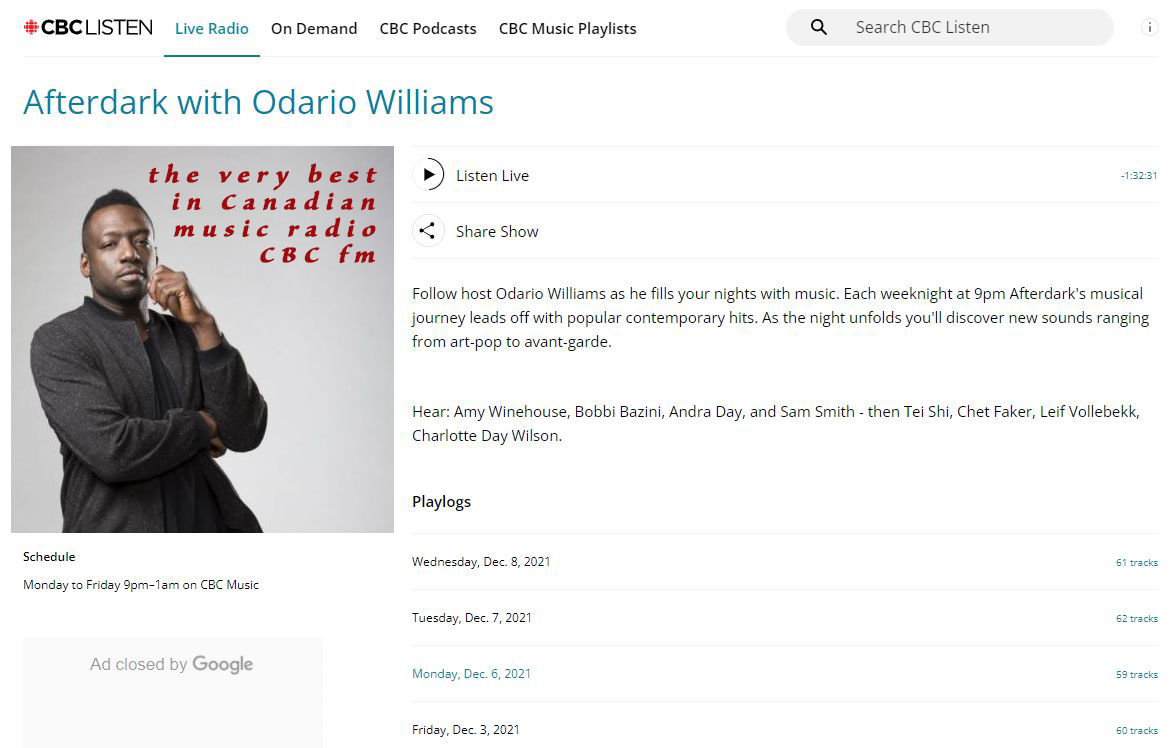
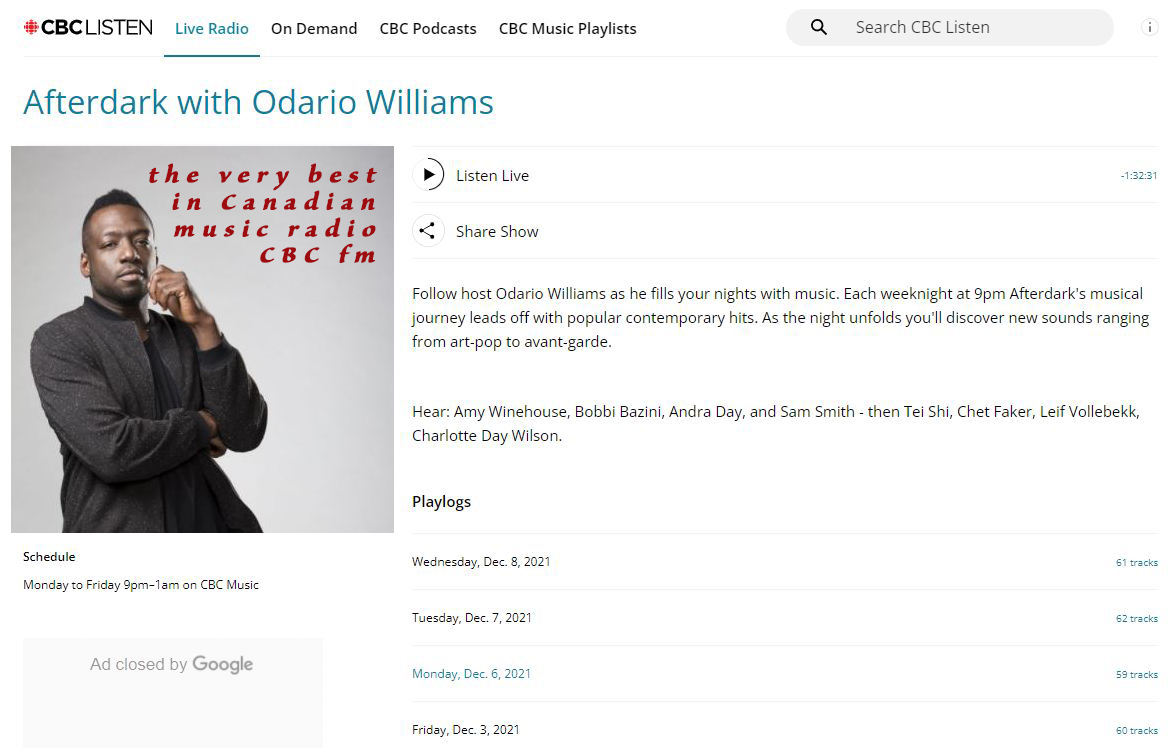
For a night time wind down and a relaxing mind set, check out CBC FM radio's AFTERDARK With Odario Williams. International music we think you will enjoy exploring is sprinkled throughout. https://www.cbc.ca/listen/live-radio/1-1051-afterdark
#afterdark #OdarioWilliams #CBCfm #radio #fm #Canada #NorthAmerica #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
People
Circles
Posts
Australia has a day time radio broadcasting to the Pacific and the world, #ABCRadioAustralia is ready to lift your spirits with the happy sounds. Just click here: https://abc.net.au/pacific/live #Australia #radio #music #Pacific #NorthAmerica #EastAsia #CentralAmerica #SouthAmerica #day #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Very best late night music radio station, we recommend, AFTERDARK With Odario Williams on CBC radio FM Canada. Fine selection of international sounds sprinkled throughout: https://cbc.ca/listen/live-radio/1-1051-afterdark #AFTERDARK #CBCfm #radio #music #Canada #world #Europe #Asia #Africa #SouthAmerica
#Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Videos
The military coup in Niger received considerable media coverage in late July, as the Presidential Guard deposed of Nigerien President Mohamed Bazoum. This coup received significant support from neighboring countries like Burkina Faso, Mali and Guinea, who like Niger, were previously under French colonial influence.
These neighboring countries have since joined a military coalition with Niger, with backing from Algeria, amid growing fears of a potential intervention by the Western-backed states in the ECOWAS coalition. Is a military confronation on the horizon? Or can this be resolved through diplomacy?
The host of The MO Manila Chan sits down with West Africa expert Koffi Kouakou to find the answers to these questions and what the future holds for Niger and the countries of the Sahel.
People
Circles
Videos
The military coup in Niger received considerable media coverage in late July, as the Presidential Guard deposed of Nigerien President Mohamed Bazoum. This coup received significant support from neighboring countries like Burkina Faso, Mali and Guinea, who like Niger, were previously under French colonial influence.
These neighboring countries have since joined a military coalition with Niger, with backing from Algeria, amid growing fears of a potential intervention by the Western-backed states in the ECOWAS coalition. Is a military confronation on the horizon? Or can this be resolved through diplomacy?
The host of The MO Manila Chan sits down with West Africa expert Koffi Kouakou to find the answers to these questions and what the future holds for Niger and the countries of the Sahel.
Posts
For a night time wind down and a relaxing mind set, check out CBC FM radio's AFTERDARK With Odario Williams. International music we think you will enjoy exploring is sprinkled throughout. https://www.cbc.ca/listen/live-radio/1-1051-afterdark
#afterdark #OdarioWilliams #CBCfm #radio #fm #Canada #NorthAmerica #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Australia has a day time radio broadcasting to the Pacific and the world, #ABCRadioAustralia is ready to lift your spirits with the happy sounds. Just click here: https://abc.net.au/pacific/live #Australia #radio #music #Pacific #NorthAmerica #EastAsia #CentralAmerica #SouthAmerica #day #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Very best late night music radio station, we recommend, AFTERDARK With Odario Williams on CBC radio FM Canada. Fine selection of international sounds sprinkled throughout: https://cbc.ca/listen/live-radio/1-1051-afterdark #AFTERDARK #CBCfm #radio #music #Canada #world #Europe #Asia #Africa #SouthAmerica
#Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
For the very best in Japanese news, social news and entertainment MIDNIGHT AT THE COFFEE SHOP recommends: TJS Radio. Just click here: https://radio.net/s/tjsradio #Japan #TJSradio #radio #Japan #NorthAmerica #Japanese #Canada #news #entertainmentNews #social
#Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Learn about the Lufthansa Airlines Malabo Office which serves as your entry point to simple travel arrangements in Equatorial Guinea. Whether you're looking to book travel or get individualized customer care, our dedicated team ensures a smooth experience. Examine practical flight schedules, gain access to exclusive offers, and get professional travel guidance customized to your tastes. For trustworthy service and comfort on every flight leaving from Malabo, choose Lufthansa.
visit website : https://airlinesofficeinfo.com/offices/lufthansa-airlines-malabo-office-in-equatorial-guinea/