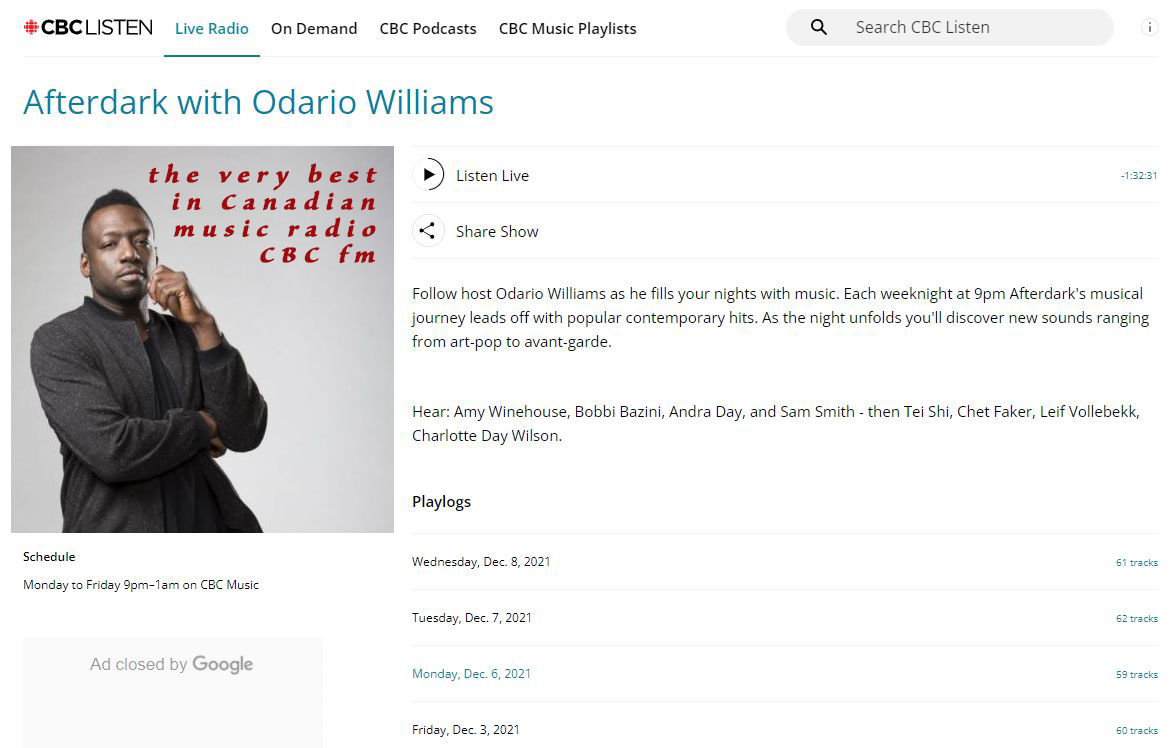
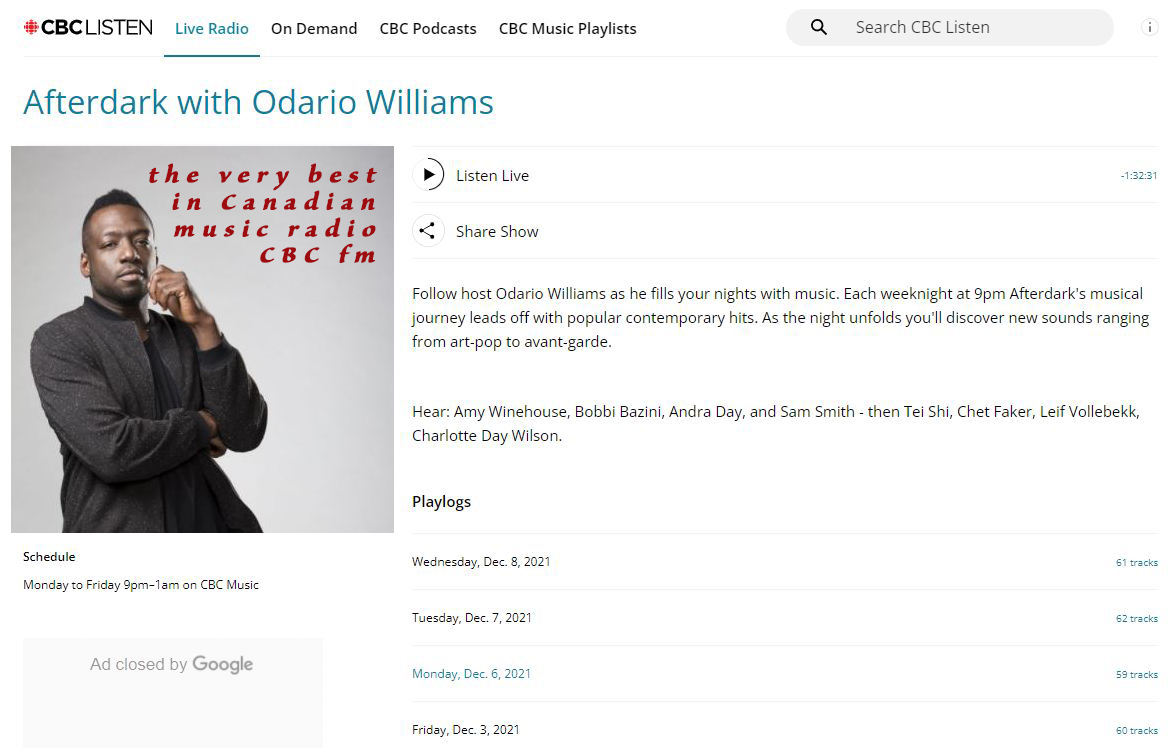
For a night time wind down and a relaxing mind set, check out CBC FM radio's AFTERDARK With Odario Williams. International music we think you will enjoy exploring is sprinkled throughout. https://www.cbc.ca/listen/live-radio/1-1051-afterdark
#afterdark #OdarioWilliams #CBCfm #radio #fm #Canada #NorthAmerica #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
People
Circles
Posts
Australia has a day time radio broadcasting to the Pacific and the world, #ABCRadioAustralia is ready to lift your spirits with the happy sounds. Just click here: https://abc.net.au/pacific/live #Australia #radio #music #Pacific #NorthAmerica #EastAsia #CentralAmerica #SouthAmerica #day #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Very best late night music radio station, we recommend, AFTERDARK With Odario Williams on CBC radio FM Canada. Fine selection of international sounds sprinkled throughout: https://cbc.ca/listen/live-radio/1-1051-afterdark #AFTERDARK #CBCfm #radio #music #Canada #world #Europe #Asia #Africa #SouthAmerica
#Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Videos
People
Circles
Videos
Posts
For a night time wind down and a relaxing mind set, check out CBC FM radio's AFTERDARK With Odario Williams. International music we think you will enjoy exploring is sprinkled throughout. https://www.cbc.ca/listen/live-radio/1-1051-afterdark
#afterdark #OdarioWilliams #CBCfm #radio #fm #Canada #NorthAmerica #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Australia has a day time radio broadcasting to the Pacific and the world, #ABCRadioAustralia is ready to lift your spirits with the happy sounds. Just click here: https://abc.net.au/pacific/live #Australia #radio #music #Pacific #NorthAmerica #EastAsia #CentralAmerica #SouthAmerica #day #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Very best late night music radio station, we recommend, AFTERDARK With Odario Williams on CBC radio FM Canada. Fine selection of international sounds sprinkled throughout: https://cbc.ca/listen/live-radio/1-1051-afterdark #AFTERDARK #CBCfm #radio #music #Canada #world #Europe #Asia #Africa #SouthAmerica
#Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
For the very best in Japanese news, social news and entertainment MIDNIGHT AT THE COFFEE SHOP recommends: TJS Radio. Just click here: https://radio.net/s/tjsradio #Japan #TJSradio #radio #Japan #NorthAmerica #Japanese #Canada #news #entertainmentNews #social
#Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe
Who is the most brilliant comedian in political history? Actually one of the few who are like George Carlin?
Check out Jimmy Dore Comedy: https://rumble.com/c/TheJimmyDoreShow?page=3
#JimmyDore #JimmyDoreShow #JimmyDoreComedy #comedy #entertainment #political #social #GeorgeCarlin #humour #funny #Afghanistan #Albania #Algeria #Andorra #Angola #AntiguaandBarbuda #Argentina #Armenia #Australia #Austria #Azerbaijan #Bahamas #Bahrain #Bangladesh #Barbados #Belarus #Belgium #Belize #Benin #Bhutan #Bolivia #BosniaandHerzegovina #Botswana #Brazil #Brunei #Bulgaria #BurkinaFaso #Burundi #CaboVerde #Cambodia #Cameroon #Canada #CentralAfricanRepublic #Chad #Chile #China #Colombia #Comoros #CongoDemocraticRepublicofthe #CongoRepublicofthe #CostaRica #CotedIvoire #Croatia #Cuba #Cyprus #Czechia #Denmark #Djibouti #Dominica #DominicanRepublic #Ecuador #Egypt #ElSalvador #EquatorialGuinea #Eritrea #Estonia #Eswatini #Ethiopia #Fiji #Finland #France #Gabon #Gambia #Georgia #Germany #Ghana #Greece #Grenada #Guatemala #Guinea #GuineaBissau #Guyana #Haiti #Honduras #Hungary #Iceland #India #Indonesia #Iran #Iraq #Ireland #Israel #Italy #Jamaica #Japan #Jordan #Kazakhstan #Kenya #Kiribati #Kosovo #Kuwait #Kyrgyzstan #Laos #Latvia #Lebanon #Lesotho #Liberia #Libya #Liechtenstein #Lithuania #Luxembourg #Madagascar #Malawi #Malaysia #Maldive #Mali #Malta #MarshallIslands #Mauritania #Mauritius #Mexico #Micronesia #Moldova #Monaco #Mongolia #Montenegro #Morocco #Mozambique #Myanmar #Namibia #Nauru #Nepal #Netherlands #NewZealand #Nicaragua #Niger #Nigeria #NorthKorea #NorthMacedonia #Norway #Oman #Pakistan #Palau #Palestine #Panama #PapuaNewGuinea #Paraguay #Peru #Philippines #Poland #Portugal #Qatar #Romania #Russia #Rwanda #SaintKittsandNevis #SaintLucia #SaintVincentandtheGrenadines #Samoa #SanMarino #SaoTomeandPrincipe #SaudiArabia #Senegal #Serbia #Seychelles #SierraLeone #Singapore #Slovakia #Slovenia #SolomonIslands #Somalia #SouthAfrica #SouthKorea #SouthSudan #Spain #SriLanka #Sudan #Suriname #Sweden #Switzerland #Syria #Taiwan #Tajikistan #Tanzania #Thailand #TimorLeste #Togo #Tonga #TrinidadandTobago #Tunisia #Turkey #Turkmenistan #Tuvalu #Uganda #Ukraine #UnitedArabEmirates #UnitedKingdom #USA #Uruguay #Uzbekistan #Vanuatu #VaticanCity #Venezuela #Vietnam #Yemen #Zambia #Zimbabwe