Prepare for possible escalation in the Middle East with lab-verified iodine supplements and a long-term storable food supply
https://bit.ly/44pQoEx
#prepping #preparedness #healthyliving #storablefood #foodsupply #stockpile #emergency #foodbucket #supplements
People
Circles
Posts
Add iodine supplements to your survival stockpile today
https://consumerwellness.store/products/health-rangers-nascent-iodine-1-fl-oz-30ml-2-strength-cap-for-long-term-storage
#prepping #SHTF #healthyliving #survival #wellness #organic #preparedness
Emergency preparedness: How to make your own activated charcoal
https://www.naturalnews.com/2022-03-14-how-to-make-your-own-activated-charcoal.html

Activated charcoal can be used for water filtration and gas masks or for treating poison. In an SHTF scenario, it would be ideal to have it on hand all the time. While making your own activated charcoal takes time, it can be done at a fraction of the cost in stores. A pound of activated charcoal […]
www.naturalnews.com
Videos
Cultural Rot And The Signs Of A Collapsing Society
>> FULL VIDEO: https://www.infowars.com/posts/cultural-rot-and-the-signs-of-a-collapsing-society/
The U.S. government’s debt has been growing at a frightening pace, elevating the importance of individual financial preparedness. As economic indicators devolve, everyone needs to focus on safeguarding their personal financial health.
Order THE CRASH COURSE here:
https://www.barnesandnoble.com/w/the-...
Wanna buy me a coffee? https://www.buymeacoffee.com/PeakPros...
Join the #1 resilience community today!
https://peakprosperity.com/membership/
ALSO FOLLOW US HERE:
Twitter: @Chris_martenson
https://rumble.com/c/PeakProsperity
https://odysee.com/@Chris_Martenson:2
People
Circles
Videos
Cultural Rot And The Signs Of A Collapsing Society
>> FULL VIDEO: https://www.infowars.com/posts/cultural-rot-and-the-signs-of-a-collapsing-society/
The U.S. government’s debt has been growing at a frightening pace, elevating the importance of individual financial preparedness. As economic indicators devolve, everyone needs to focus on safeguarding their personal financial health.
Order THE CRASH COURSE here:
https://www.barnesandnoble.com/w/the-...
Wanna buy me a coffee? https://www.buymeacoffee.com/PeakPros...
Join the #1 resilience community today!
https://peakprosperity.com/membership/
ALSO FOLLOW US HERE:
Twitter: @Chris_martenson
https://rumble.com/c/PeakProsperity
https://odysee.com/@Chris_Martenson:2
Posts
Prepare for possible escalation in the Middle East with lab-verified iodine supplements and a long-term storable food supply
https://bit.ly/44pQoEx
#prepping #preparedness #healthyliving #storablefood #foodsupply #stockpile #emergency #foodbucket #supplements
Add iodine supplements to your survival stockpile today
https://consumerwellness.store/products/health-rangers-nascent-iodine-1-fl-oz-30ml-2-strength-cap-for-long-term-storage
#prepping #SHTF #healthyliving #survival #wellness #organic #preparedness
Emergency preparedness: How to make your own activated charcoal
https://www.naturalnews.com/2022-03-14-how-to-make-your-own-activated-charcoal.html

Activated charcoal can be used for water filtration and gas masks or for treating poison. In an SHTF scenario, it would be ideal to have it on hand all the time. While making your own activated charcoal takes time, it can be done at a fraction of the cost in stores. A pound of activated charcoal […]
www.naturalnews.com
Sprouts: Your perfect emergency preparedness food choice
https://www.naturalnews.com/2024-03-13-sprouts-perfect-emergency-preparedness-food-choice-prepping.html
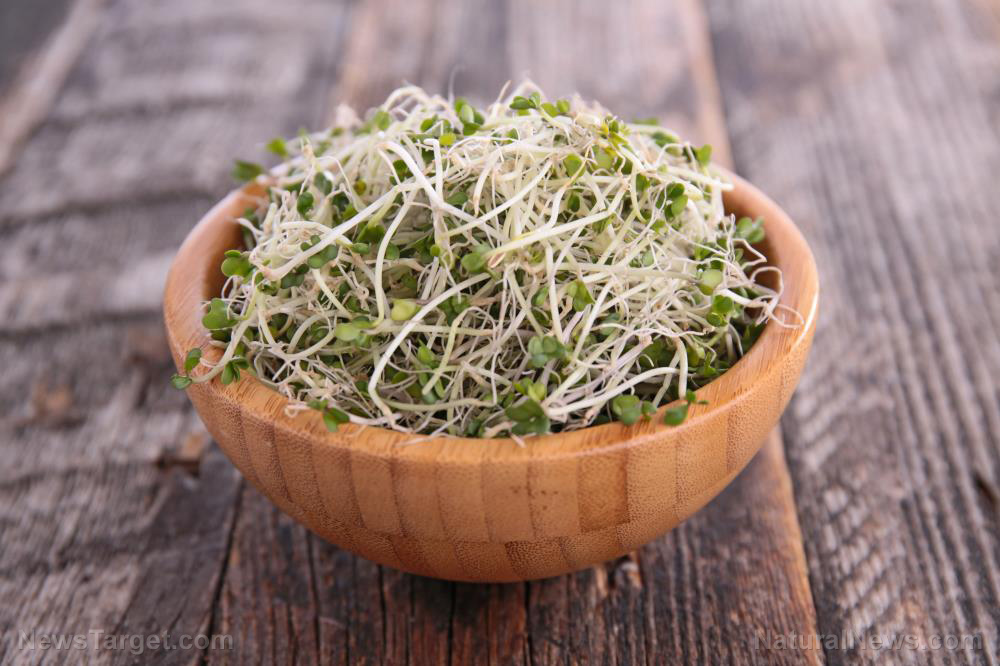
For a newbie prepper, deciding which food items to stock up on can be overwhelming. If you’re not sure where to start, focus on stockpile staples like canned food, dried foods and nutritious items like sprout powders. Starting your prepper stockpile before SHTF ensures that your family has access to shelf-stable, nutritious food when things […]
www.naturalnews.com
Emergency preparedness: How to make your own activated charcoal
https://newstarget.com/2022-03-14-how-to-make-your-own-activated-charcoal.html

Activated charcoal can be used for water filtration and gas masks or for treating poison. In an SHTF scenario, it would be ideal to have it on hand all the time. While making your own activated charcoal takes time, it can be done at a fraction of the cost in stores. A pound of activated charcoal […]
www.newstarget.com










