For secular Jews given THAT exhibitedly careless & clearly clueless HONOR via God ie: HIS chose people despite Gentiles 70 centuries-2 date have had-having 2 pick up slack (unsuccessfully & me no better than NO 1) for THEM? But hey, eternal glory, misc B to 3 in 1-1 in 3 Holy Trinity. MAY B cuz of Holy Bible's Genesis 11:7 as 1 mere example aside from other's ie: Exodus 32 & Matthew 21:12. & separately else - Harry Potter author Joanne Kathleen Rowling; she wrote: War is Peace. Freedom is Slavery. Ignorance is Strength. Her comments were a nod to George Orwell's 1984. Huh OH how the UGH of 2 date (after 70 centuries) NEVER ceases 2 ill amaze, misc me. STUPID no even cut it.
People
Circles
Posts
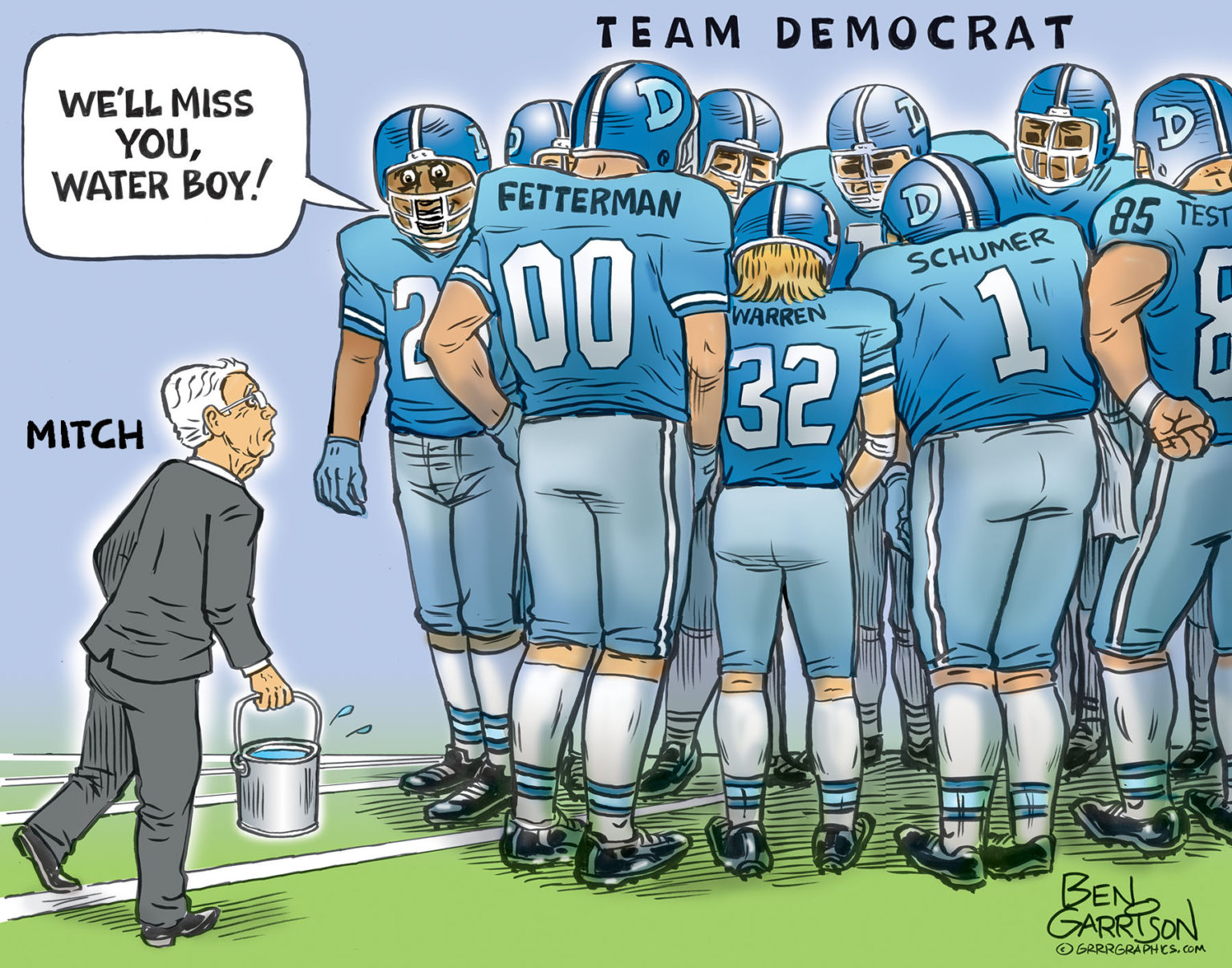
MITCH MCCONNELL, THE DEMOCRAT WATER BOY
Cartoon published 02/29/2024
Mitch McConnell announced that he will be resigning from his Senate leadership position, but not until November.
While his announcement triggered celebration from the America First crowd, we at GrrrGraphics ask…why wait til November? Step down NOW, Mitch—why wait? At 82 years of age, you’re not getting any younger. Oh, but we almost forgot…he moves slowly because after all, he’s known as ‘The Turtle.’
McConnell will give up his leadership roll, but he plans on serving out the rest of his senate term which ends in 2027. Mitch will be 85 then. Judging by his declining health, will he even make it to the end of his term? It’s ridiculous how these geriatrics ‘serve’ in office until they drop dead. Maybe it’s because they like the power and self-enrichment. We need term limits! Mitch has had multiple ‘freezing’ events involving a blank stare into space lasting many seconds. One time his aides for forced to whisk him away from the podium. Like Joe Biden and the late Senator Feinstein, Mitch’s senior moments are now commonplace and expected. He should step down and completely retire from the Senate.
Mitch, as a Uni-party RINO, has carried the water for the Democrats for decades. He was elected to the Senate in 1984, when the US debt was $1.572 trillion. Under his long watch it’s now $34 trillion. Some conservative, huh? He’s one of many Republicans who stabbed Trump in the back. Meanwhile, Fox News has been praising Mitch up and down, leaving us shaking our heads in disagreement. Fox news is controlled by the Uni-party, so that is to be expected.
Rep. Matt Gaetz (R-Fla.) said “better days are ahead for the Republican Party” after McConnell’s announcement. Congressman Bob Good chimed in with, “Mitch McConnell stepping down provides a great opportunity for true conservative leadership in the Senate. Senator Rick Scott would make a great Republican leader.”
An better choice would be Senator Rand Paul. A true Constitutionalist and America first warrior, Rand has the experience and the iron will to lead the Senate.
Senator John Cornyn (TX) has thrown his hat in the ring for the leadership position.
We don’t need another Uni-Party RINO Republican leader whose main concern is preserving the Swamp and carrying water for the Marxist Democrats.
— The GrrrTeam
Videos
In 1984, George Orwell portrayed in chilling detail how totalitarian governments use the power of language to manipulate the masses. This notion was not unfamiliar to the founders, as James Madison warned that changing definitions of words over time would create “a metamorphosis” that would destroy the original limitations of the Constitution.
Path to Liberty: April 27, 2023
JOIN TAC: https://tenthamendmentcenter.com/members/
Show Archives: https://tenthamendmentcenter.com/pathtoliberty/
Subscribe and Review on Apple: https://podcasts.apple.com/us/podcast/path-to-liberty/id1440549211
In 1984, a Senator from Delaware who now lives in the White House helped create the federal civil asset forfeiture program known as “equitable sharing.” Learn what it is, how it works, and how it’s used to circumvent state restrictions on asset forfeiture, which is legalized government robbery.
Path to Liberty: March 9, 2022
JOIN TAC: https://tenthamendmentcenter.com/members/
Show Archives: https://tenthamendmentcenter.com/pathtoliberty/
Subscribe and Review on Apple: https://podcasts.apple.com/us/podcast/path-to-liberty/id1440549211
Circles
Videos
In 1984, George Orwell portrayed in chilling detail how totalitarian governments use the power of language to manipulate the masses. This notion was not unfamiliar to the founders, as James Madison warned that changing definitions of words over time would create “a metamorphosis” that would destroy the original limitations of the Constitution.
Path to Liberty: April 27, 2023
JOIN TAC: https://tenthamendmentcenter.com/members/
Show Archives: https://tenthamendmentcenter.com/pathtoliberty/
Subscribe and Review on Apple: https://podcasts.apple.com/us/podcast/path-to-liberty/id1440549211
In 1984, a Senator from Delaware who now lives in the White House helped create the federal civil asset forfeiture program known as “equitable sharing.” Learn what it is, how it works, and how it’s used to circumvent state restrictions on asset forfeiture, which is legalized government robbery.
Path to Liberty: March 9, 2022
JOIN TAC: https://tenthamendmentcenter.com/members/
Show Archives: https://tenthamendmentcenter.com/pathtoliberty/
Subscribe and Review on Apple: https://podcasts.apple.com/us/podcast/path-to-liberty/id1440549211
Posts
For secular Jews given THAT exhibitedly careless & clearly clueless HONOR via God ie: HIS chose people despite Gentiles 70 centuries-2 date have had-having 2 pick up slack (unsuccessfully & me no better than NO 1) for THEM? But hey, eternal glory, misc B to 3 in 1-1 in 3 Holy Trinity. MAY B cuz of Holy Bible's Genesis 11:7 as 1 mere example aside from other's ie: Exodus 32 & Matthew 21:12. & separately else - Harry Potter author Joanne Kathleen Rowling; she wrote: War is Peace. Freedom is Slavery. Ignorance is Strength. Her comments were a nod to George Orwell's 1984. Huh OH how the UGH of 2 date (after 70 centuries) NEVER ceases 2 ill amaze, misc me. STUPID no even cut it.
MITCH MCCONNELL, THE DEMOCRAT WATER BOY
Cartoon published 02/29/2024
Mitch McConnell announced that he will be resigning from his Senate leadership position, but not until November.
While his announcement triggered celebration from the America First crowd, we at GrrrGraphics ask…why wait til November? Step down NOW, Mitch—why wait? At 82 years of age, you’re not getting any younger. Oh, but we almost forgot…he moves slowly because after all, he’s known as ‘The Turtle.’
McConnell will give up his leadership roll, but he plans on serving out the rest of his senate term which ends in 2027. Mitch will be 85 then. Judging by his declining health, will he even make it to the end of his term? It’s ridiculous how these geriatrics ‘serve’ in office until they drop dead. Maybe it’s because they like the power and self-enrichment. We need term limits! Mitch has had multiple ‘freezing’ events involving a blank stare into space lasting many seconds. One time his aides for forced to whisk him away from the podium. Like Joe Biden and the late Senator Feinstein, Mitch’s senior moments are now commonplace and expected. He should step down and completely retire from the Senate.
Mitch, as a Uni-party RINO, has carried the water for the Democrats for decades. He was elected to the Senate in 1984, when the US debt was $1.572 trillion. Under his long watch it’s now $34 trillion. Some conservative, huh? He’s one of many Republicans who stabbed Trump in the back. Meanwhile, Fox News has been praising Mitch up and down, leaving us shaking our heads in disagreement. Fox news is controlled by the Uni-party, so that is to be expected.
Rep. Matt Gaetz (R-Fla.) said “better days are ahead for the Republican Party” after McConnell’s announcement. Congressman Bob Good chimed in with, “Mitch McConnell stepping down provides a great opportunity for true conservative leadership in the Senate. Senator Rick Scott would make a great Republican leader.”
An better choice would be Senator Rand Paul. A true Constitutionalist and America first warrior, Rand has the experience and the iron will to lead the Senate.
Senator John Cornyn (TX) has thrown his hat in the ring for the leadership position.
We don’t need another Uni-Party RINO Republican leader whose main concern is preserving the Swamp and carrying water for the Marxist Democrats.
— The GrrrTeam
What this Bill C63 leads to is if you write anything in Canada, YOU, as a journalist or author, will require a Liberal Party censor to give his Liberal Party "okay" on your work in order for it to be ALLOWED to be in print: https://www.youtube.com/watch?v=62mCx74M11w #censorship #LiberalParty #Canada #Bill63 #dictatorship #authors #articles #law #1984 #hatespeech #PrimeMinister #insane #insanity #war #revolution #future #crime #thoughtcrime #communism #JimmyDoreShow #LeeCamp #GeorgeGalloway #ChrisHedges #Redacted #KimIversen #MarkSteyn #RevolutionaryBlackOutNetwork #GarlandNixon #DanBongino #TheGrayZone #JacksonHinkle #RusselBrand #Wikileaks
Thursday, February 8th, 2024
What Is a Culture?
Dr Naomi Wolf
America 2.0: Taxation Without Representation
Donald Jeffries
Why I’m Interviewing Vladimir Putin.
Tucker Carlson
FBI Raids of Safe Deposit Boxes
Doug Casey
One of These Things Is Not Like the Others
George F. Smith
Who Owns the gold?
Alasdair Macleod
The EU Wants Reparations For Ukraine Paid By Russia
Helena Glass
2024 Is the New 1984: Big Brother and the Rise of the Security Industrial Complex
John & Nisha Whitehead
From Rule Britannia To Decrepit Old Bulldog
Finian Cunningham
Is Zinc Deficiency Behind the Dramatic Spike in Yeast Infections?
Dr. Joseph Mercola
Gazacaust: Placing the Blame Where It Belongs
Ron Unz and Mike Whitney
The Nord Stream Pipelines and the Perils of Containment
Seymour Hersh
https://www.lewrockwell.com